Bilirubin is a pigment found in bile that is mostly formed during the breakdown of hemoglobin. We understand why it is important to measure it.
Don't store avocado like this: it's dangerousLa bilirubin is a pigment found in bile and which is formed for the most part during the destruction of hemoglobin, contained in red blood cells that are damaged or have finished their life cycle. Because it is important to measure it? And what does it entail to have high bilirubin?
Its name derives from the particular reddish-yellow color: in fact the word comes from the union of the Latin bilis, bile, with the word ruber, red. After being produced, bilirubin arrives in the liver to then be expelled from the body, especially through the faeces and only in small part in the urine.
Index
What is bilirubin
Bilirubin is a reddish-yellow substance that represents the main component of bile and whose production is linked to the process of destruction of senescent red blood cells, that is, of those who have exhausted their life cycle.
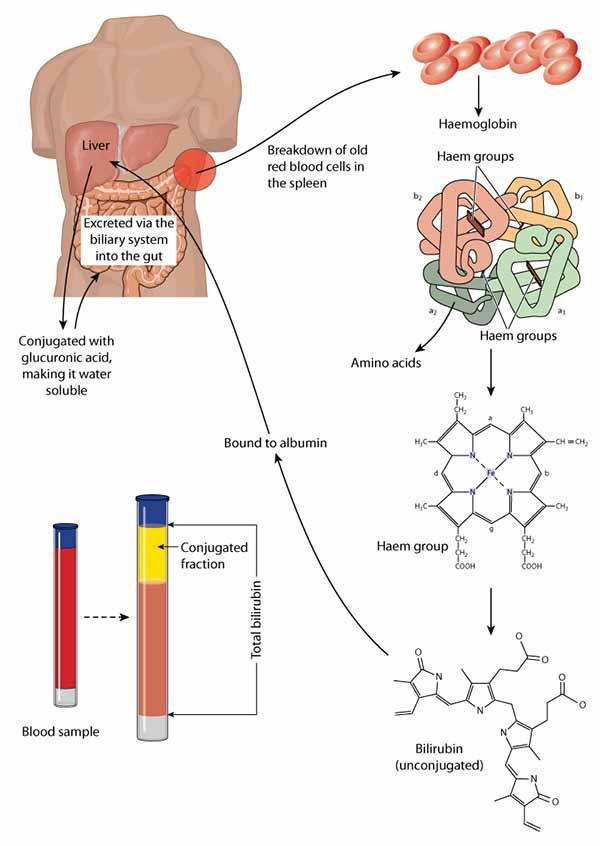
Bilirubin is produced, in fact, above all from the demolition of old or damaged red blood cells inside the endothelial reticulum system (a functional system of the body characterized by three types of cells: reticular located in the lungs, spleen, bone marrow and lymph nodes; macrophages and Kupffer cells, which are found in the liver). Instead, one fifth of bilirubin production is from lead back to the catabolism of serum haemoproteins, that is, it derives from the demolition (lysis) of other hemoproteins (myoglobin, cytochromes, peroxidase, catalase) and erythroblasts (for anomalies that occur during the synthesis of red blood cells in the bone marrow, see ineffective erythropoiesis).
READ also: HIGH OR LOW CREATININE. REFERENCE VALUES AND HOW TO REGULATE IT
Bilirubin, therefore, is one waste substance of our organism deriving from the normal breakdown of hemoglobin, the protein that is found in our red blood cells, and is at the same time one of the components of bile.
Once produced, bilirubin it arrives in the liver and is subsequently excreted from the body, mainly through the disastrous but also with urination. Based on this disposal process, two types of bilirubin are distinguished. This disposal activity occurs in the cells of the reticuloendothelial system of the spleen, liver and bone marrow. Macrophages are found here that are able to recognize aged red blood cells and thus engulf them. In this way they free hemoglobin which divides into its protein part and into the heme group from which bilirubin is degraded.
This is the so-called bilirubin "frees it" or "not conjugated", Or also defined"live". It is in this case insoluble, whereby to be transported must rely on a serum protein produced by the liver, thealbumin. With albumin, unconjugated bilirubin reaches the liver where it detaches from albumin and is conjugated with glucuronic acid resulting in the formation of direct or conjugated bilirubin.
If all these bilirubin excretion processes do not work, a buildup of bilirubin in the blood may occur (iperbilirubinemia) and in tissues, inducing the so-called jaundice, due to which the skin has a yellowish tint.
Reference values and why to measure bilirubin
To represent a good diagnostic criterion for evaluating the state of health of the liver is precisely the relationship between direct bilirubin and indirect bilirubin: the share of total bilirubin produced every day is around 250 mg and reaches an average concentration of 1-1,5 mg / dL in the blood.
The values may change depending on the laboratory to which one refers, but usually the “physiological” total bilirubin is brought back in the range between 0.3 and 1.0 mg / dl.
La direct bilirubin oscillates between 0.0 and 0.4 mg / dl. There indirect bilirubin ammonta a 0.1 e 1.0 mg / dl. (Fonte: Inran)
To recap:
0.3-1.0 mg/dl, total bilirubin
0.1-1.0 mg / dl, bilirubin free
0.0-0.4 mg / dl, conjugated bilirubin
But always refer to the data from your analytical laboratory.

Bilirubin is measured by the normal blood tests and its detection can be influenced by certain factors, such as the intake of certain drugs, a particular diet or intense physical exertion. Also there pregnancy it may slightly increase the direct bilirubin values, while in non-pregnant women and children it tends to settle on values a little lower than normal.
Detection of bilirubin by analysis is usually prescribed for certain reasons:
- monitor the health of the liver and the progression of particular diseases, such as hepatitis
- understand if the red blood cells are destroyed too quickly compared to the normal process and thus diagnose a possible one
- haemolytic anemia
- identify the causes of jaundice in a newborn
- evaluate the possible toxicity of a particular drug treatment and the efficacy of a particular therapy
- understand if the bile ducts are blocked
High bilirubin, when to worry
Typically, bilirubin levels higher than the physiological level (iperbilirubinemia) are a symptom of pathologies or a liver malfunction. However, it is necessary distinguish between an increase in indirect or free bilirubin and an increase in direct or conjugated bilirubin: for this reason, thefractional examination of bilirubin.
If the concentration values are particularly high (equal to 2.5 - 3 mg / dl), it is in the presence of a jaundice (the main symptom of which is the yellowish color of the skin and sclerae of the eyes). Depending on the affected area, jaundice is divided into:
- prehepatic (increased bilirubin production)
- hepatic (liver dysfunction)
- post-hepatic (obstruction of the ducts)
Hyperbilirubinemia of the unconjugated type
Frequent in newborns is the increase in free or indirect bilirubin that can also be found in the case of hemolytic diseases (due to the shortening of the average life of red blood cells in circulation), when the increase in the production of bilirubin due to the increased breakdown of red blood cells exceeds the ability of the liver to metabolize it.
Conjugated hyperbilirubinemia (hepatic or hepatocellular jaundice)
Instead, it is due to the reduced uptake of bilirubin by the hepatocyte, to reduced conjugation with glucuronic acid or reduced excretion with bile, due to hereditary genetic syndromes such as Crigler-Najiar syndrome or the Gilbert's syndrome.
THEexcess of total bilirubin, but above all indirect, it can be caused by:
- Gilbert's syndrome
- reaction to transfusions
- haemolytic or pernicious anemia
- cirrhosis
READ also: HIGH TRANSAMINASIS: CAUSES, SYMPTOMS AND FOODS TO AVOID
If the Conjugated bilirubin has higher levels than unconjugated bilirubin, usually means that the liver cells are unable to eliminate bilirubin as well as possible. And this can be mainly caused by:
- viral hepatitis
- alcoholic hepatitis
- reaction to certain drugs
It can also happen there conjugated (direct) bilirubin is higher than unconjugated (indirect) bilirubin due to an obstruction of the bile ducts, which occurs in:
- presence of bile duct stones
- presence of lesions of the bile ducts
- presence of tumor
Finally, the increase in bilirubin may be due to rare hereditary diseases which cause an abnormality in the metabolism of bilirubin. In this case the syndrome in Rotor, of Dubin-Johnson and Crigler-Najjar.
Neonatal hyperbilirubinemia and jaundice
Usually, excess bilirubin in infants should not cause concern because it absolutely is temporary and clears up on its own in a couple of weeks at the most. However, it can be cured with one phototherapy or special medications and, only in the most serious cases, with a blood transfusion.
Excess can be caused by breakdown of red blood cells faster than normal, but there may be other causes such as:
- congenital infections
- hypoxia
- several genetic diseases
- liver disease

In most cases, only unconjugated or indirect bilirubin increases, while an increase in conjugated or direct bilirubin can occur in case of rare diseases such as biliary atresia or neonatal hepatitis.
In any case always evaluate the consultations with your pediatrician and all the tests to be done, to determine whether it is physiological jaundice, not indicative of a disease, or pathological.
In summary, we are in the presence of physiological jaundice se:
- appears 48-72 hours after birth
- it resolves spontaneously
- the increase in bilirubin occurs slowly and gradually
- bilirubin values do not exceed a certain threshold (12 mg / dl in term newborns)
- the color of stool and urine is normal
Low bilirubin
Generally, a low bilirubin value in a healthy person does not indicate abnormalities and must not cause alarm. In healthy people, the main causes of bilirubin are:
- an excess of vitamin C
- caffeine
- some anticonvulsant medicines (such as phenobarbital) and some medicines to treat lung disease, such as theophylline which, like caffeine, contains xantine which reduce bilirubin levels
In some studies, low bilirubin levels are associated with conditions such as:
- coronary artery dysfunction
- seasonal depression
- haemolytic anemia
- terminal stage of chronic kidney disease
On the pathologies associated with altered blood values you can also read:
- CREATINE: PROPERTIES, SIDE EFFECTS AND THINGS TO KNOW BEFORE TAKING IT
- HOMOCYSTEINE: WHY IT IS SO IMPORTANT TO KEEP VALUES AT BOTTOM
In all cases, it always is better to consult your doctor and identify your general clinical picture.
Germana Carillo